
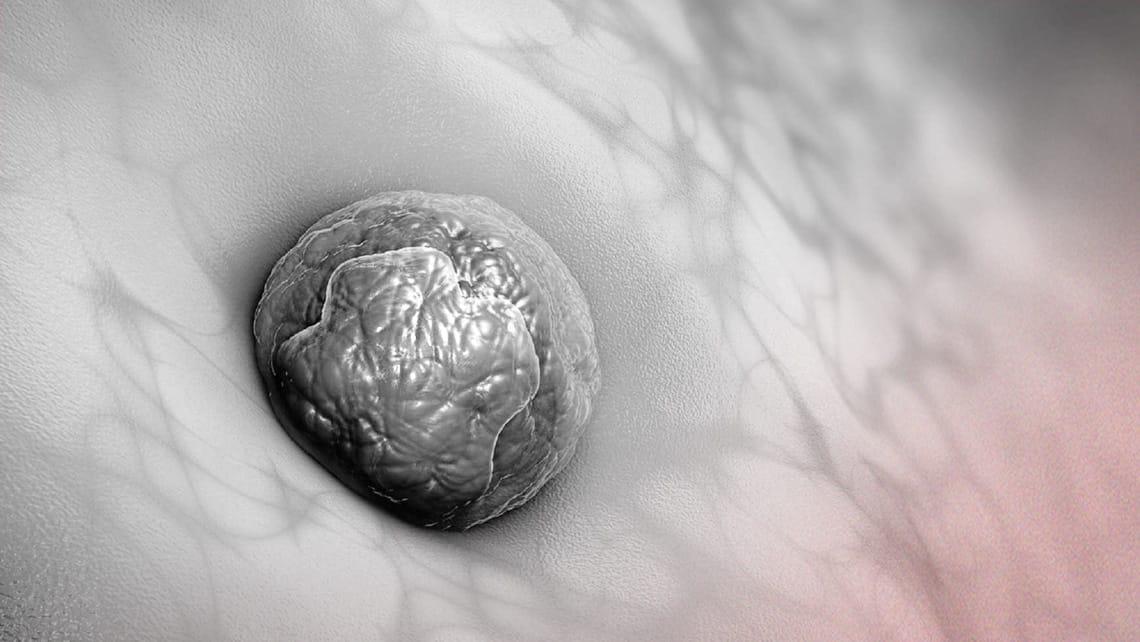
In the world of surrogacy, embryo transfer is often seen as a hopeful milestone. But when implantation fails, it can be emotionally exhausting and medically puzzling. While embryo quality and timing are well-discussed, one often-overlooked factor is immunological rejection — the surrogate’s immune system reacting against the embryo.
What Is Immunological Implantation Failure?
Implantation failure occurs when a healthy embryo, placed in a receptive uterus, does not attach or grow. In some cases, this is due to the body mistakenly treating the embryo as a “foreign object.” This can happen even if the uterus looks structurally healthy.
Common Immunological Factors
- Elevated Natural Killer (NK) Cells: While NK cells normally fight infections, elevated levels in the uterus may attack the embryo.
- Th1/Th2 Cytokine Imbalance: A skewed immune response can prevent implantation or lead to miscarriage.
- Autoimmune Disorders: Conditions like lupus or Hashimoto’s can trigger systemic inflammation harmful to early pregnancy.
- Antiphospholipid Syndrome (APS): This clotting disorder increases miscarriage risk and can affect implantation.
Diagnostic Tools
- Endometrial biopsy to measure NK cell activity.
- Blood tests for inflammation markers (e.g., ANA, cytokine panels).
- HLA testing to assess immune compatibility.
- ERA (Endometrial Receptivity Analysis) to evaluate uterine timing.
Available Treatments
Although controversial and not guaranteed, some treatments have shown promise:
- IVIG (Intravenous Immunoglobulin): Modulates immune response to be more pregnancy-friendly.
- Intralipid Infusions: A lower-cost alternative to IVIG that may suppress overactive NK cells.
- Steroids (e.g., Prednisone): Temporarily reduce inflammation and immune attack.
- Heparin or Aspirin: Used when blood-clotting risks are present (especially in APS cases).
What Surrogates and IPs Should Know
- Personalized care matters: Immune-related failures require specialized reproductive immunology consultation.
- Repeated implantation failure (RIF) should not be dismissed — ask for further testing if two or more transfers fail.
- Emotional support is essential: When the body says “no,” it’s not your fault. Surrogates need empathy, not blame.
Conclusion
Understanding the body’s immunological response opens new possibilities for improving embryo transfer success in surrogacy. The more we uncover about this complex system, the better we can protect the emotional and physical wellbeing of surrogates — and the dreams of intended parents.
